Being a good parent is not about how you feed your baby. There is only one rule. Feed your baby. In other words, to put it very succinctly:
Fed is best.
There are plenty of very good reasons why some moms don’t nurse. And guess what, you don’t even need to justify your decision to anyone. But for any mom who wants to and is physically able to breastfeed, this post is for you.
Breastfeeding has documented benefits for both the mother and the baby. It also has the advantages of convenience (your breasts are always with you, the milk is the perfect temperature and you don’t need to clean anything) . I am not sure if you have looked at the price of formula lately, but you can add the bonus of significant cost saving
Goodness, I even have moms apply breastmilk to eyes, nose and rashes. It has almost magical properties.
But nursing is also hard work! It is the rare mom who has a completely easy time with it. Just because it is a natural process does not mean that there is anything about it that actually feels ‘natural’! Especially during the first 2 weeks when the body is adjusting and unless you are in the vast minority, there is often quite a bit of discomfort.'
Note to partners and family members:
When mom complains about pain or feeling overwhelmed, the correct response is “I am proud of you for doing this, let me know how I can support you” not “Well you can stop whenever you want.”
The myriad of strong opinions can add to the frustration.
Julie Hartman, Certified Lactation Counselor, new parent educator and birth doula feels passionately that breastfeeding education before the baby is born can be the key to a successful start.
She speaks to so many moms with a similar refrain: “I am going to try to breastfeed and see how it goes but I am open to options if it gets hard.”
Julie’s response is “I don’t want too many frustrated tears from the baby or from mommy, but let’s see if we can set you up for success. If you can, give yourself a solid two weeks before changing course. Get support from a lactation professional to help get over the bumps.”
For some moms it might be longer than 2 weeks. The key is don’t be too quick to give up.
While getting some education in advance is ideal, having some hands-on coaching once the baby arrives can also make a big difference. Most hospitals have in-house lactation support. Unfortunately sometimes you need to be your own advocate and ask for the help if it isn’t automatically offered.
Our goal with this post is to give moms information and resources that are useful for those essential first two weeks and beyond.
What is the genesis of this document?
For three years, Dr. Ted and I worked together at a startup called Oath Care. The company was created to support people with many different aspects of parenting. This included lactation guidance.
While neither of us are lactation experts, he and I spent several months putting together a comprehensive guide to make sure that all Oath’s lactation consultants were on the same page and updated with all of the current data. Alas, the Oath Care app shut down in December of 2023, but I dug out our guidelines a couple of months later to share with my daughter when she had her second child. She found it useful, and thus we wanted to share it more widely.
We are so lucky to have Julie Hartman add her wisdom to this document.
Dr. Ted, Nurse Judy, and Doula/CLC Julie’s Breastfeeding Resource
Purpose
The online lactation world can be an intense and polarizing place. There are millions of opinions, all of them equally loud, and it can be hard to discern what’s real for a breastfeeding parent. Similarly, lactation consultants may have differing practices, and may give conflicting advice to breastfeeding parents without context. This is oftentimes based on their wisdom from decades of practice. Our mission is to combine practical wisdom and experience with the most current data.
How to use this guide
Below is a brief section on general breast care, which applies to everybody who choses to breastfeed, followed by a collection of suggestions on oft-controversial individual topics. We also tried to cover issues that many moms end up dealing with,
We have listed the series of topics in alphabetical order, most with a brief primer, the upside and downside of the issue (both sides to the argument), and our final perspective on the topic. Links included in this document are all public access, with the exception of the 2022 Breastfeeding Medicine Guidelines above. Please note that there is rarely a “right answer” to any topic, so if our perspective seems vague, that’s why. We are attempting to strike a balance between opposing sides.
Master some basic techniques
First Droplets has some good introductory videos and information that focuses on the first hours of breastfeeding.
Learn a hold that is comfortable, for you and baby. Once you’re back from the hospital, many find the side-lying position allows mom to rest while the baby feeds. Some babies will have preferences for one side over another based on how they were positioned in the womb. The lazier the better!
General Breast Care
This section has information that should apply to every parent that chooses to breastfeed (as opposed to the below topics that aren’t universally applicable).
Rubbing expressed milk on nipple and areola and allowing it to air dry: heals microscopic wounds, has antibodies, anti-inflammatory properties, etc.
Breasts should be completely dry before putting on a shirt or bra.
Avoid scents: Don’t use scented soaps or creams on the breast area.
Nipple pain management: most parents experience some amount of discomfort, at least in the first couple weeks of feeding.
Preventative: Ensure a good deep latch. This is the one and only thing that can circumvent pain completely over time. Some recommend the “flipple” technique”.
Products: Silverettes and bamboo breast pads are often helpful to most parents regardless of their situation. Anecdotally, orally taking sunflower lecithin oil can be helpful (more on this below).
Know that this is mostly normal, and there’s an end in sight. Zingy, zappy, electric nerve pain in the first couple days to weeks of consistent breastfeeding is not unexpected. It should only last 30 to 90 seconds. Anything more than that should be checked.
These things are normal
Night sweats. Mild night sweats not associated with a fever are explained by normal hormonal changes.
Cramping and subsequent vaginal bleeding when nursing in the first weeks postpartum
New body smells. Think teenager with adolescent BO.
Nipples getting darker and larger. Once again this is nature at its finest. The darker nipples make it easier for the babies to find their target.
Breasts are not necessarily equal. One might produce more than the other. In Lauren’s case, one seemed to produce more than the other (slacker boob and hero boob) She named them accordingly: Her left breast was squirty. Her right was called drippy. When you wean you may even notice that they are very different sizes. This generally normalizes.
Slightly higher temperature. When breastfeeding, your body will generally feel more heated because of the extra work you are doing and the closeness of the baby.
Reminder: The following topics are listed in alphabetical order. For ease of use, you can try Cmd + F or Ctrl + F to quickly search the document with key words.
Blebs
What are they: From Dr. Katrina Mitchell – “Blebs, inflammatory lesions on the surface of the nipple orifice, reflect underlying ductal inflammation and microbiome disruption with biofilm formation. They may be described as ‘blisters’ or ‘scabs.’ Patients also may describe ‘shards,’ ‘stones,’ or ‘pebbles’ being expressible from their nipples. This is all ductal debris, like a storm gutter getting congested with leaves that eventually float down the stream. While uncomfortable, they aren’t harmful or dangerous. Continually ‘expressing’ these little ‘pebbles’ is not healthy for the breast tissue nor for mom’s mental health.”
Upside: N/A
Downside: N/A
Our Perspective: Do not “unroof” or in any way manually manipulate nipple blebs. Breast tissue is fragile and inflicting trauma will not be helpful and may create scar tissue. Blebs can be painful but often go away on their own. Old recommendations used to be for warm Epsom salt soaks, but breastfeeding experts such as Dr. Katrina Mitchell, MD recommends strongly against them due to the risk of damaging the skin in her article Blebs Mythbusters.
Julie Hartman, CLE, recommends dangle feeding.
Blood in Poop (and Dairy Elimination)
What is it: Blood in the diaper, usually within the first 4 months, can be a finding that occasionally requires an intervention or change. It can feel like an alarming finding, but small amounts of blood are very common.
Our Perspective: As a general rule, any well-appearing infant can have a bloody poop once. If they continue to be happy, feed, and the blood seems like specks or less than a quarter-size, parents can continue to feed without making changes (and check for irritation around the anus to see if that’s a cause). If there is significant fussiness, refusal to feed, or repeated blood, it’s worth thinking about a dietary change, such as a full dairy elimination for mom if breastfeeding, or a formula change to something like Elecare/Alimentum or another hydrolyzed formula.
Blood in Spit Up
What is it: Spit Up that is pink-tinged or has frank red blood can be an alarming finding. However, in an otherwise healthy baby, this is usually caused by maternal blood in mom’s nipples. Evaluate the baby and the nipples. If the baby is happy and feeding well, this is a mom problem. Consider lanolin, Vasoline, or other nipple ointments.
Body Mechanics
We’re breaking the format to emphasize this point: Take care of your body.
When I worked at a pediatrics office I would often come into the waiting room where a mom was nursing in an awkward position
“Would you like a nursing pillow?”
“No, I’m fine.”
“No you’re not… Here is a pillow.”
“Ah, wow, that is so much better.”
Mamas, PLEASE, take care of your body. Sitting hunched over with everything flexed is going to take a toll. Use support pillows when you are nursing. There are many. I am a fan of My Brest Friend nursing pillow. Other pillows do not clip and stay close to mom’s body, and therefore the baby’s weight can push the pillow away from contact with the mom and cause poor positioning of the baby on mom’s body.
During feedings, make sure your body, shoulders, and neck are supported. The baby should be placed high enough on mom’s body (with the support of the pillow) so that she is not hunching or slouching forward. The baby should come to you, not you to the baby.
In between feedings, make sure you stretch! There are lots of resources online for nursing moms that have some specific exercises for your neck, shoulders and wrists. Don’t wait until you have an injury!
Bras
What are we talking about: Bra fit is subjective to a person’s comfort. But also, there are completely contradicting opinions out there, easily found on social media. According to some providers, the tightness of a bra may or may not impact breast swelling and success of breastfeeding.
Upside: A well-fitting and supportive bra, such as a tighter sports bra, may help to decrease breast swelling and minimize mastitis, particularly for heavy breasts.
Downside: According to la leche league, a bra that puts too much pressure on your breasts may result in sore breasts due to congested and swollen ducts or decreased supply. It’s important to note that this assertion has not been proven by any scientific evidence.
Our Perspective: Wear what you’d like. The breasts are engorged and edematous in the first 6 weeks after birth. A more supportive bra may be beneficial for people with heavy breasts because they help to decrease fluid buildup in the breasts. This seems to be more important when mom is upright, less so when lying down. Ultimately, your choice should be yours for comfort. Alternatively, if you're having trouble with clogs, be on the lookout for underwires, cross-body bag straps or other things that might be causing focal pressure points. A tight-fitting bra might be a tool for you when trying to wean because it might suppress milk production.
Burping
What is it: Burping is the process of sitting a baby up after a feeding and patting them on the back. This allows babies to move excess gas bubbles out after a feeding.
Upside: Some babies seem more comfortable after burping. They might have less reflux symptoms and less spit ups. Formula-fed babies might benefit more from burping than exclusively breastfed babies, because formula is not as physiologic.
Downside: Not every baby needs to burp. Burping might unnecessarily wake a sleeping baby and cause them to look like they’re hungry, when in fact they’re just annoyed from being woken up.
Our Perspective: There’s no one-size fits all, trial and error is needed. Burping is not 100% necessary, but may be helpful for formula-fed babies, babies with reflux, babies with colic, and moms with an oversupply or robust milk supply. There is also no specific amount of time that every baby needs for burping.
Cow’s Milk Allergies, Blood in Poop, and Avoiding Milk in Breastfeeding
What is it: “Food protein-induced allergic proctocolitis of infancy” (FPIAP) refers specifically to red blood with or without mucus in the stool of otherwise healthy infants, usually within the first 2 months of life. In exclusively breastfed infants, this is thought to be due to proteins in the mother’s diet. It has been suggested that breastfeeding moms eliminate the offending agent to improve the symptoms (in 76% of cases, this is cow’s milk, less often egg and soy).
Upside: Some research and guidelines have demonstrated that simple elimination of the offending agent will, over up to 2 weeks (but often less than that) resolve the symptoms.
Guidelines: https://pubmed.ncbi.nlm.nih.gov/22569527/
Review article: https://pubmed.ncbi.nlm.nih.gov/21134576/
Downside: Others argue that there is no connection, and there are some studies that suggest that in 99% of babies with cow’s milk allergies, there is not sufficient allergen in the breast milk to cause a reaction. https://jamanetwork.com/journals/jamapediatrics/article-abstract/2764081
Our Perspective: It’s hard to ignore the large body of research and anecdotal evidence. We suggest that it is simple enough to trial an elimination diet in patients with blood in the stool to see if there is improvement, despite the conflicting data.
Dream Feeding
What is it: Many meanings, but the general gist is “feeding babies while they remain sleeping.” This might be done with breastfeeding, bottle feeding pumped milk, or bottle feeding formula.
Upside: In the 0-3 month range, overnight feedings are very acceptable ways to keep babies calm and sleeping long stretches of time while still getting essential nutrients. Proponents argue that babies evolved to bedshare and sleep overnight while still very sedated.
Downside: After around 3-4 months of age, when patterns and skills are being learned due to the advancement of the infant nervous system, dream feeding causes babies to associate feeding with falling asleep. This might further ingrain bad habits and will make sleep training more difficult, if sleep training is desired.
Our Perspective: Dream feeding is physiologic and expected at very young ages (such as below 3 months). After 3-4 months, parents that wish to eventually sleep train their babies will find it advantageous to have taught babies to always fall asleep on their own, in a crib/bassinet. However, sleep training is a personal choice and will not impact health so long as growth remains appropriate.
Engorgement
What is it: Engorgement can be painful and is a balancing act. The first milk that is produced is called colostrum. It is rich in essential nutrients for the newborn. In about 3- 5 days the actual breast milk typically comes in. In some cases, it can do this with a vengeance. Many moms wake up shocked to find that their breasts are suddenly enormous, warm, tender and very firm. The goal is comfort and adequate milk supply. The risk of pumping is stimulating oversupply.
Julie suggests that you stay away from the pump in favor of having the baby at the breast to relieve any discomfort and begin regulation. It may help to hand express until the breast is soft enough for the baby to get a deep latch. Things will regulate over time as your body and the baby figure things out.
Our perspective: Any form of nipple stimulation, be it breastfeeding or pumping, will send messages to the brain to stimulate milk production. This may be desired in the setting of low supply, but if there is excessive engorgement it may exacerbate the issue. A very small amount of pumping between feedings can be okay in very limited circumstances, but BAIT (breast rest with ice/NSAIDs, see Mastitis) is preferred to avoid overstimulation.
“Flat/Inverted” Nipples and the Use of Nipple Shields
What is it: Some nipples may appear “flat” or “inverted.” This may be due to having large breasts, or breasts that are swollen from IV fluids in delivery or just regular anatomy. Many of these parents are told to use a nipple shield to help their baby latch.
Upside: Nipple shields can be tools used to assist with breastfeeding. Some moms find them more comfortable during breastfeeding because they protect from overstimulation and soreness, and they can decrease some of the pain sensations described above. They may help to assist with latch in the early stages of breastfeeding.
Downside: Nipple shields make a layer of distance between a baby’s mouth, which decreases direct stimulation of nipple skin by baby. This might decrease supply. Nipple shields are rarely completely necessary, and telling new mothers that they need nipple shields can contribute to them feeling like failures at supporting their child. Nipples are smooth muscular tissues which can become erect with stimulation, allowing for the creation of a protuberant nipple. See photo:

Our Perspective: They are given out way too frequently in hospitals. While nipple shields may be useful temporary tools, they are not physiologic. Nipple shields should be used when under the care of a lactation professional who can guide you and wean you from the shields when you’re ready. They can be helpful, but with proper coaching, ideally moms can get to the point where they can nurse without a nipple shield. If you’re going to use them, provide your baby with some extra mouth to skin time on the breast.
Freezer Stashes
What is it: Extra pumping to create a large “stash” of frozen breast milk, often designed for when moms return to work or as an insurance policy if mom finds she can’t breastfeed.
Upside: Breast milk is the gold standard for feeding your child. Babies often tolerate it well, and are used to the taste.
Downside: Encouraging such overpumping can risk mastitis and blebs for moms, and in moms with low supply can create anxiety. There is some data to suggest that freezing milk over a long period of time can decrease its total fat content, which babies need (although this is small, likely 14% over 3 months). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3411345/
Our Perspective: Being an excellent mom is not about the milk. Remember:The only rule is feed your baby. It is okay if it isn’t exclusively breast milk. We suggest breastfeeding when it works for mom but do not think moms should stress about having a stash in the freezer. At some point it is beneficial to have some options for if supplementation is needed for any number of reasons.
Pro tip
Make sure you date your containers of milk and use the oldest ones first.
To make sure your freezer hasn’t had any periods where it hasn’t maintained the correct temperature, put a small baggie of ice cubes in the back. As long as the ice cubes maintain their shape, you can be assured that nothing has been warm enough to melt.
Here is the CDC guidelines for breastmilk storage.
Galactogogues
What are they: Galactagogues refer to foods, herbs, or medications that are believed to increase the production of breast milk. They have been used for centuries to increase breast milk supply in parents that have low supply issues. Dr. Katrina Mitchell does a wonderful job summarizing all galactagogues here, but the food and herbal examples are excerpted below:
Food Galactagogues
Common examples of food galactagogues also called lactogenic foods include things such as:
Oatmeal. Oatmeal is a good source of iron and we know that low iron levels in breastfeeding women can impact milk supply. Having a nice warm bowl of oatmeal for breakfast using just half a cup of dry oats can provide nursing moms with about 20% of their daily iron requirement.
Garlic. After consuming garlic, some studies have shown that babies breastfeed longer. This could be why garlic is considered a galactagogue because more breastfeeding can lead to increased milk supply.
Fennel seed. These liquorice-flavored seeds have long been used by women to make more milk likely due to compounds in fennel that are similar to estrogen.
Green leafy vegetables. They are full of nutrients like calcium as well as phytoestrogens which might have a boosting effect on breast milk production.
Malt. Like from Guinness Beer. Some lactation consultants have had great success with this! You can also find malt powder in the grocery store. Or just drink some Ovaltine.
Herbal Galactagogues
There is not a lot of research on how herbal galactagogues work. It is believed that they have a boosting effect on prolactin levels which in turn increase milk supply.
Fenugreek. This is one of the most well-known and often used herbal galactagogues.
Milk thistle. Long linked to breastfeeding, milk thistle is believed to help milk supply due to its plant estrogens.
Goat’s rue. From the same plant family as fenugreek, goat’s rue is believed to stimulate growth in breast tissue and milk production.
Blessed thistle. It’s believed that blessed thistle stimulates lactation by boosting prolactin and oxytocin levels which in tandem help increase milk supply and release it from the nipples.”
Upside: While some galactagogues have their risks, most galactagogues, particularly foods, are extremely low risk, and may help. Galactagogues are small things that breastfeeding parents can choose, and may help augment the work being done by lactation consultants to increase supply.
Downside: Despite being used for centuries, modern science has not been able to reliably produce research demonstrating significant increased production of breastmilk by galactagogue use. In addition, most galactogogues are not approved by the FDA for breastfeeding purposes, and as such are not monitored for efficacy or safety in that setting. It has also been shown that the amount of dietary supplements in a product can vary widely, so it’s not clear that customers are getting what they pay for (it may be too much or too little). Additionally, some practitioners fear that focus on galactagogues can distract parents from doing more proven interventions for increasing supply, such as breastfeeding frequency and latch work.
Our perspective: There is risk and benefit to everything in breastfeeding. There are certain interventions that might be considered helpful to milk production that are known to be safe with no downside. These include eating iron-rich foods, leafy green vegetables, and garlic. Most moms tolerate fennel as well. However, careful consideration needs to be given to herbs and medications. If patients are having real trouble with milk supply, they need to seek individual medical attention. Also keep track of the baby's growth. If they are staying on the growth curve, you are doing fine!
Hindmilk / Foremilk Balance
What is it: Foremilk refers to the carbohydrate-rich milk that settles in the front of the breast after time has passed from the last feed. Higher fat-content milk has a tendency to settle in the back of the breast, away from the nipple (referred to as ‘hindmilk’). A ratio of more foremilk to hindmilk can contribute to discomfort and explosive stools in infants due to the high lactose content of the foremilk. However, it is most important to recognize that this “imbalance” can occur in combination with hyperlactation (oversupply) or lots of time passing between feeds. Addressing oversupply or fully draining the breast with a feed can help. It is also important to know that this hindmilk/foremilk factor does not contribute to poor infant weight gain.
Our Perspective: There’s no real upside or downside as this isn’t much of an argument. La Leche League has a great primer on foremilk and hindmilk here. Most moms never need to think about the balance of foremilk and hindmilk, because the breast naturally regulates the distribution of fats and carbs in the milk, as they write. For parents that are seeing lots of mucousy green poops (lots might mean more than 8 stools per day PLUS the color/consistency issues), this could be an indicator that the balance is off for your baby. These parents should consider fully emptying one breast before moving onto the other.
Hyperlactation (Oversupply of Milk)
Having too much milk can be as much of a struggle as not having enough. Yes, there are some boobies that go way overboard and some moms make way too much milk in the beginning. Eventually things will even out. Try to avoid building more supply. Ice and cabbage leaves might help. Avoid pumping.
Icky Feeling When Breastfeeding (“DMERs”)
What is it: A poorly understood medical phenomenon, there is a hypothesis that some breastfeeding parents experience a profound neurochemical imbalance during breastfeeding. It’s been described as awful and visceral. The only well studied treatment has been SSRI medication. “Just powering through” has not been an effective treatment for these parents.
Our Perspective:if a parent describes strong consistent negative emotions when nursing, pay attention. This may be DMERs, a condition which is commonly undiagnosed but which can respond to SSRI, so follow up with MD is indicated.
(If you found this by looking up the word’ icky’ alphabetically then you get 100 points🙃)
“Insufficient Glandular Tissue”
What is it: Some parents that do not make enough milk are told that they might have “insufficient glandular tissue.”
Our Perspective: This term oversimplifies a complicated and nuanced issue for breastfeeding mothers. We prefer the term hypolactation, because the word “insufficient” implies a failure by the body of the mother. In some cases supplementation is necessary. We aim to support a parent’s desire to breastfeed, but the only actual rule is to feed your baby.
Latch
What is it: “Latch” refers to the position and stability of the baby’s mouth on a breast.
Upside: Proper positioning can help with transfer of milk and minimize pain. A note on pain: quantifying pain in the newborn period is tricky. Pain is subjective, and some discomfort might be expected in the first 2-4 weeks. Little tweaks can still make a huge difference in this discomfort, so it’s still important to reach out for help if you’re unsure.
Downside: Talking about latch in this way can reinforce the idea that there is such a thing as a “perfect latch.” This is not helpful nor is it accurate. Nipples and mouths come in many different shapes and sizes, and an effective transfer of milk may look different from breast to breast.
Our Perspective: “Perfect” techniques and perfect nipples are not realistic nor required. All that matters is that the baby is getting milk and mom is not in immense discomfort.
Legal Rights
You are allowed to nurse in public! Be aware that all 50 states have laws that allow women to breastfeed in public or private places. The specifics of the laws may vary state by state, if you are interested in reading the statutes specific to your state, you can find those here.
For pumping moms: the Fair Labor Standards Act (FLSA) requires employers to provide reasonable break time for an employee to express breast milk for their nursing child for one year after the child's birth each time such employee has need to express the milk. Employees are entitled to a place to pump at work, other than a bathroom, that is shielded from view and free from intrusion from coworkers and the public.
It’s reasonable to demand more than a closet. If your employer isn’t providing at least running water, you may want to consider talking to HR.
“Lipase (High Lipase)” Milk
What is it: Lipase is an enzyme that breaks down fat into fatty acids that are present in breast milk. There is a hypothesis that some parents have milk with higher concentrations of lipase. According to this hypothesis, when this milk is frozen and then thawed, the milk can have an odor due to the compositional changes in the milk (the lipase continues to break down fat, even when frozen, and broken down fat smells sour). Some babies will reject this milk.
Upside: There’s no safety issue with this milk. Milk that has been appropriately frozen and then thawed is safe to drink regardless of a change in smell. Scalding the milk by heating it in a saucepan until it comes to a quick boil and stopping it will break down lipase and stop the milk from changing smells in the freezer. This would need to be done before freezing the milk.
Downside: There are many providers that do not believe that lipase variability and activity in milk is possible. Furthermore, the heating of milk does destroy antibodies, which are one benefit of breastfeeding (although calories matter more).
Our Perspective: Before you make a freezer-full of milk, you may choose to freeze one batch of milk for at least 2 weeks to see if this is a problem. If the baby takes the milk, then there is no need to fret. If you end up having milk that has this issue, Julie has a great hack. A drop of alcohol free vanilla extract ( trader Joes has it) will often make the baby drink it down without complaining.
Massaging
What is it: Historically, lactation guidelines taught that milk could become “plugged” in ducts, and that would cause discomfort and occasionally mastitis. (Note: “plugged” milk isn’t really a thing, see below for more.) The teaching was that massaging a breast could coerce the plugged milk out. Massage by hands and devices, such as electronic toothbrushes or other vibrating things, used to be recommended.
Upside: Many historical guidelines suggest gentle massage towards the nipple to “clear plugged ducts.”
Downside: These historical guidelines are not based on any consistent data proving that massage of the breast resolves mastitis. Ample anecdotal evidence shows that deep massage of the breast can worsen mastitis and inflict trauma on the breast tissue.
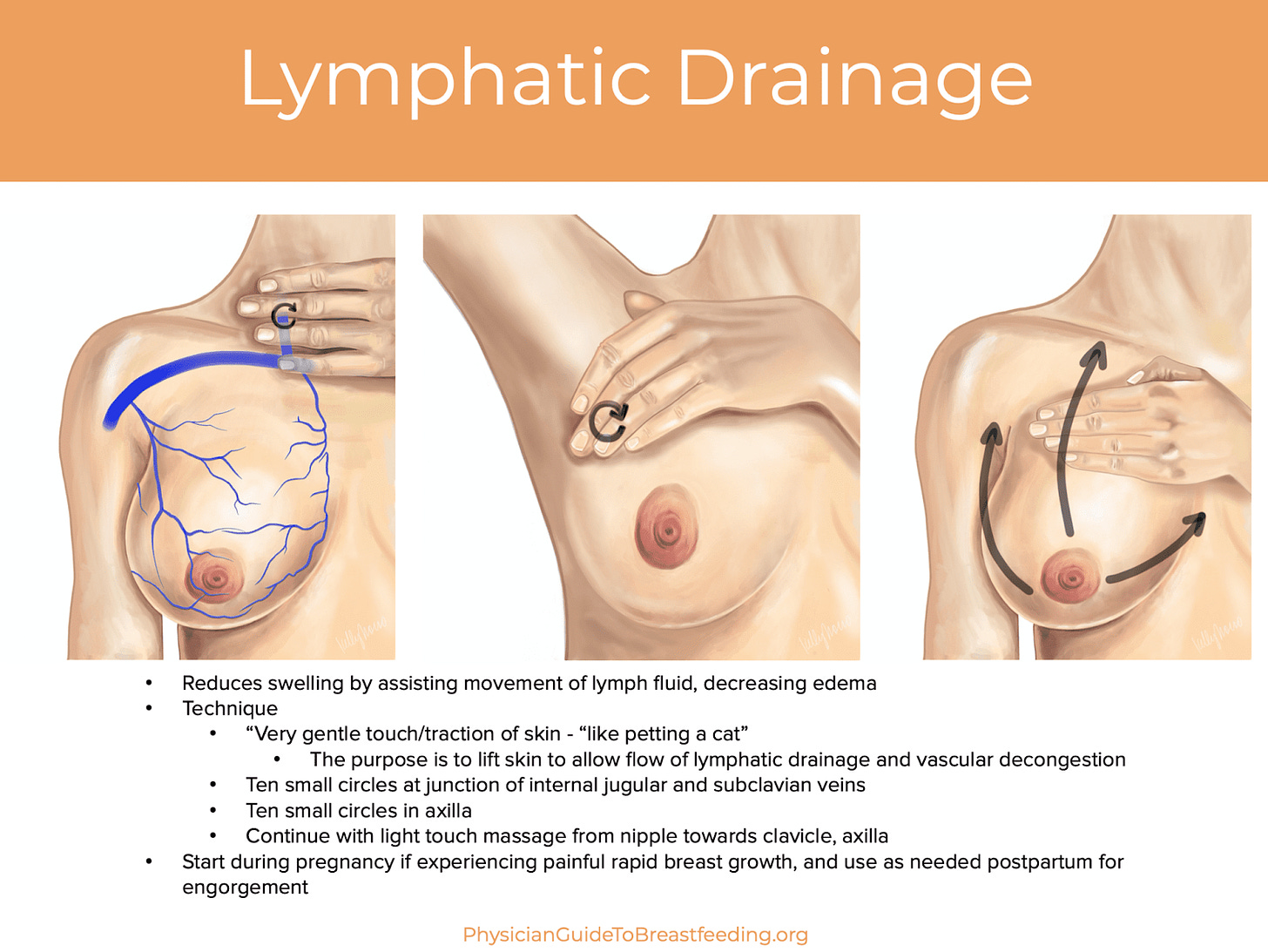
Our Perspective: Gentle lymphatic massage (lightly brushing fingers over the skin to lift skin off the breast tissue to drain fluid), pictured below, can help to reduce swelling and improve mastitis. Deep massage of the breast is not recommended, and may cause harm. Electric toothbrushes or other devices are not recommended.
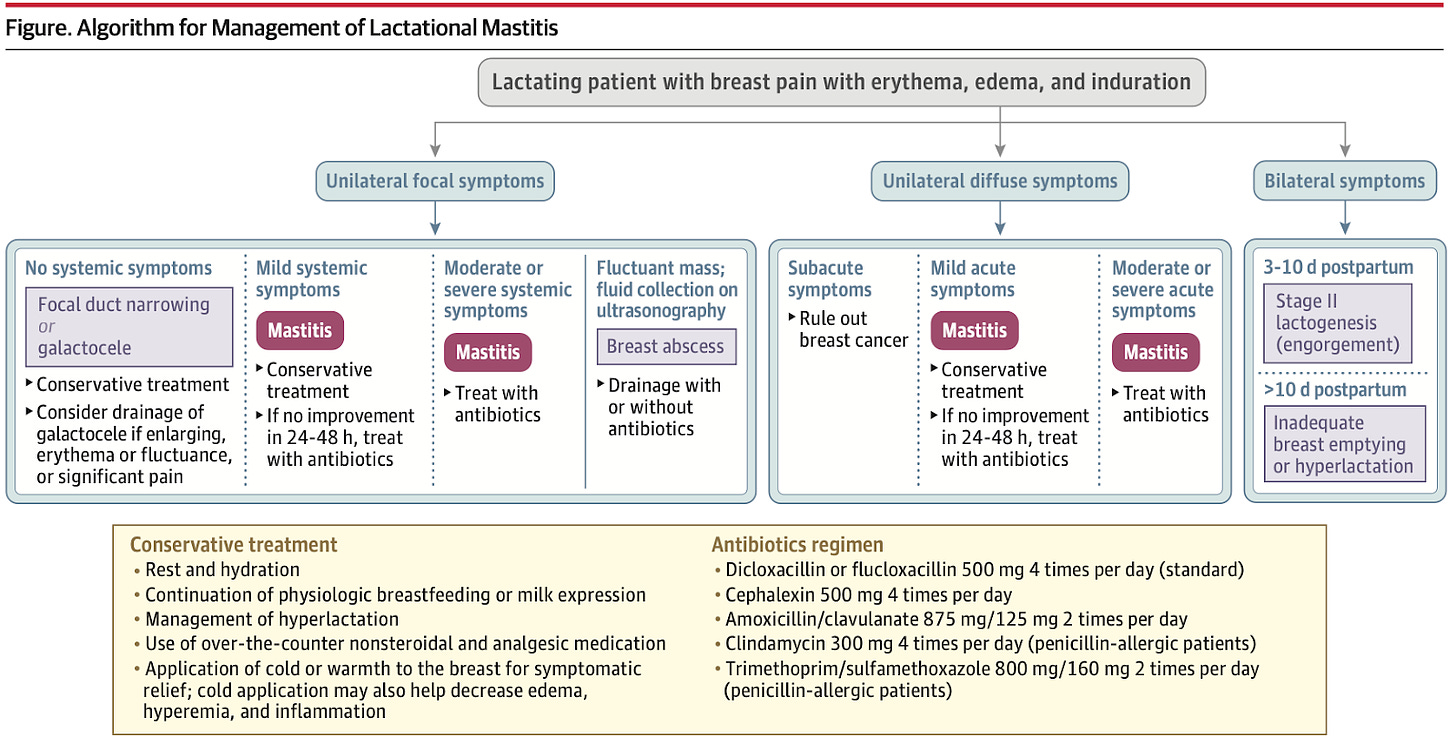
Mastitis Protocol
One of the most important drivers behind this document is the treatment of mastitis, inflammation of the breast. Treatment can vary widely from provider to provider. The 2022 protocol for mastitis is illustrated below in an article from JAMA. Major changes from the previous guidelines are outlined below the illustration.
Major Changes
The above guidelines represent a reversal from the old first-line guidelines for early mastitis. Some of the most commonly employed interventions from the old guidelines are listed below:
Apply warm compresses to the breast or take a warm shower.
Breastfeed frequently, starting with the affected breast.
Use a pump to express milk between feedings.
Massage the breast area.
The new guidelines are almost the opposite:
Apply ice to the breast. Warm compresses might make things worse.
Continue to breastfeed, but do not favor the affected breast; in some cases, use only the unaffected breast.
Minimize breast pump usage; do not “pump to empty” the breasts.
Avoid deep massage of the breasts (if any massage is needed, use light lymphatic drainage only [instructions above]).
Pro Tip: Ice application can be tricky. Some breastfeeding moms like the gentle use of an “ice roller” to cool an engorged or painful breast. Make sure the device you use is smooth, not studded or vibrating.
The Science Behind the Change
It’s important to understand the science and studies that led to the current change in guidance. There has been a shift in our understanding of early lactational mastitis. While it was previously believed that things like clogged ducts were responsible, and could be milked or massaged through, it is now understood that swelling and inflammation of the glands and ducts of the breasts themselves, and the surrounding tissue, are to be blamed for the pain/swelling and even low-grade fevers. With resting the breasts, icing them, or engaging in “physiologic breastfeeding” (i.e. feeding only what is needed, not pumping to drain the breast), symptomatic improvement can happen without the need for further interventions.
Why did massage work in the first place and why the change?
Many lactation consultants have had success using breast massage in the past, so these recommendations are an adjustment. It’s important to note that every breast is unique. As we reviewed above, easing interstitial fluid (fluid outside of the ducts) will help to decrease inflammation and improve the physiologic flow of milk. Some breasts are resilient to traumatic forces (pushing on the glands) and are not impacted by massage. In fact, massage may have worked to decrease excess interstitial fluid in some breasts. However, studies have shown that massage risks damaging underlying tissue and may make some swelling worse. Since the goal is to decrease inflammation, rest, ice, and only feeding what baby needs will work to do that without the risks of tissue aggravation with massage.
Does massage help a clogged duct?
More on this above, but the research has moved away from the idea that mastitis arises from single clogged milk ducts. Ducts are microscopic and interconnected, like a spider web, so a small amount of congested milk in any single duct will usually not create painful symptoms (there is such a thing as a galactocele, but they’re more rare than we previously thought). Only a specific form of massage, lymphatic drainage, has been shown to improve outcomes for mastitis. Lymphatic drainage is tricky, it’s a specific light stroking of the skin that is difficult to perfect without hands-on training. Because it’s so difficult to perform without guidance, it is not generally recommended as a first-line intervention. Read more about lymphatic drainage above.
Mastitis: Antibiotics
What is it: Mastitis is a painful inflammation of breast tissue that often affects breastfeeding women. Symptoms can include pain, swelling, warmth, and redness in the affected breast that sometimes includes a breast infection that can also cause fever and chills. It’s important to note that the “itis” refers to inflammation, and while infection may sometimes cause the inflammation in mastitis, not all mastitis is an infection. In fact, most early mastitis, especially without fevers or chills, are not infections.
Upside: If infectious mastitis has been diagnosed, antibiotics may be prescribed for a 10-day course and are generally very effective at treating the problem.
Downside: There is concern that overuse of antibiotics may upset the gut microbiome, lead to drug-resistant bacteria, and come with some side effects. It generally takes about 3 days or more for a true skin infection to develop, so many providers believe that we are too quick to move to antibiotics for breastfeeding parents with initial symptoms.
Our Perspective: Antibiotics should almost never be the first-line treatment for patients with early mastitis. Patients should go first to BAIT (breast rest, advil, ice, tylenol), not massage or aggressive “draining” of the breast. Warmth is okay for occasional comfort. Antibiotics can and should be discussed after 24 hours of significant symptoms such as chills/fevers over 101.5, significant redness in a “wedge” distribution on the breast, and worsening pain/tenderness.
Mastitis, Products
What are they: At the first sign of mastitis, Nurse Judy has anecdotally seen improvement with the use of Happy Ducts (and Sunflower or Soy Lecithin, see more on that below). Happy Ducts is a mix of herbs that purport to improve lymphatic flow around the breasts and facilitate milk movement through the ducts. They’re taken as a dietary supplement a couple times per day for a short while.
Mastitis, Recurrent
What is it: Recurrent mastitis does not have a universally accepted definition, but may be considered as any repeating episodes of mastitis (fever, breast redness, breast swelling, and/or breast pain). There is no upside/downside here, but certain considerations need to be made for appropriate treatment.
Our Perspective: We agree with the 2022 Academy of Breastfeeding Medicine Guidelines: Confirm that the correct antibiotics were completed for the correct amount of time. Change antibiotics if a full course was recently completed, and work up recurrent mastitis with medical specialists trained in breastfeeding medicine (consider ultrasound/imaging and other interventions). Check with your doctor or read more below about sunflower or soy lecithin as one more thing you can try.
Maternal Diet (does cabbage or dairy make your baby fussy?):
What is it: This is not an entry on blood in the poop (already done, see above about dairy or milk in the maternal diet). There are some anecdotal reports that maternal diet can impact a baby's comfort. As an example, eating broccoli, garlic, coffee, or dairy.
Upside: Mild dietary tweeks in mom can make the baby seem more comfortable by producing less gas.
Downside: One could make the argument to parents to power through by not eliminating food. Babies' comfort levels go up and down all the time, and temporary discomforts may spontaneously resolve without forcing moms to suffer by restricting their diet. Dr. Ted’s perspective: Babies are going to grow up to eat many of the things their parents eat, and introducing those things early could help young guts to adjust. We know this happens in adults. We don’t have data to support this specifically in newborns.
Our Perspective: It’s sad to watch your baby in discomfort, but if the discomfort is mild and there’s no blood in the stool, this is a personal choice. There is no study to show that fussiness in a baby from mom’s diet is causing any harm. As such, there is no medical reason to eliminate coffee or cabbage from the maternal diet, so long as babies are growing and happy. But if breastfeeding parents notice that babies are repeatedly upset only when moms are drinking coffee, mom can make her own judgment call about whether or not to cut out her morning cup.
In Nurse Judy’s case cabbage was a clear offender and it wasn’t such a hardship to do without it. We understand that skipping coffee is much more of a sacrifice.
Night Time Feed Spacing
Baby is sleeping longer stretches on their own? Hooray for you! You have made it to the point where the baby is ready to space out some of those overnight feedings. Remember: the magic of breastfeeding works on supply and demand. We need to train your body to not wake up when the baby no longer needs milk at night. The best way to do this is by gentle expression. Pumping will cause your body to expect more milk production overnight and may do the opposite of what is intended.
If your baby is still waking up to feed, moms do still need to remove milk from their body one way or another, either by baby breastfeeding or mom pumping.
Nursing strike / Baby temporarily refuses to nurse
What is it: If your baby or toddler has been breastfeeding well and suddenly refuses to nurse, it is possibly what is called a “nursing strike.” Nursing strikes are temporary.
Here are some of the biggest culprits and things to try:
Change in your supply
Have you been ill? Out in the hot sun and possibly dehydrated? On any new medications? Some antihistamines can have a drying impact on your supply.
What can you do?
Make sure you are drinking plenty.
Minimize optional medications that could be the culprit. If you are dealing with allergies, try nasal irrigation rather than antihistamines.
Do lots of skin to skin contact.
Try nursing while moving (using wrap or carrier).
If there is one feeding that is especially frustrating, consider pumping for that one and having a partner or support system offer a bottle.
Baby health
Is the baby teething? Is there any congestion or signs of illness or ear infection?
What can you do?
Try different positions to see if some are more successful.
If the baby is teething, you can try some of these remedies.
If the baby is fussier than normal for several days it is worth getting them checked.
Is the baby distracted?
Right around four months is a common age for this. There are enormous developmental changes going on. You might find that they pop off the breast or bottle more frequently to pay attention to their surroundings. (god forbid they should miss anything)
What can you do?
Try nursing in a quiet, dark room. Put on some soft music or white noise.
Personal note from Nurse Judy:
I feel you if you are dealing with this. Don’t give up like I did. I stopped nursing my first child at 4 months because I didn’t have support getting over the hump.
Most of the time this is temporary. If you want to keep nursing, don’t let this stop you.
Placental Encapsulation
What is it: Processing placenta for birthing parents to ingest. (no, we are not kidding, this is a thing).
Upside: It is thought to improve outcomes for postpartum depression. Anecdotally, we have occasionally seen this to be true.
Downside: The placenta is necessarily full of the hormone progesterone. Progesterone (“Pro-gestation” – i.e. promotes “gestation,” which is infant growth in the womb) works against lactation.
Our Perspective: Placental encapsulation may decrease milk supply. For some parents, this isn’t a problem (people with a large supply or hyperlactation). For the others who want to breastfeed but do not have an over-abundant supply, it can be problematic.
“Plugs”
What are they: Historically, it was thought that soreness in the breast could be a result of a “plugged duct,” a duct in the breast that was blocked up with a thick piece of milk.
Our Perspective: This is a confusing concept because many decades of lactation advice included the directive to “massage a plug” out by compressing the breast towards the nipple. We have come to learn that this is not true because the network of ducts below the nipple are too numerous and interconnected to become meaningfully plugged just by thickened milk. In reality, the sensation of a “plug” is just swelling and pain around an area of ducts, but should be treated with breast rest, ice, and over-the-counter pain medications if needed. If any massage is to be used, it should be gentle lymphatic drainage as pictured above.
Probiotics for Babies Only
What are they: Probiotics are bacteria given to babies to help balance the microbiome of the gut. The newborn microbiome is seeded by many things, including the act of vaginal birth or breastfeeding, which pass the parental microbiome on to the offspring.
Upside: Proponents of probiotics believe that even babies born vaginally to breastfeeding parents may be receiving a microbiome that has been disrupted by generations of antibiotics and might benefit from an added probiotic. We have seen improvement in things like diaper rash and colic with the use of some probiotics.
Downside: Probiotics can be expensive, another thing to worry about, and may not be necessary in every baby. Some babies that seem gassy or fussy might just be ingesting air or have a parent with over-supply of breastmilk, and probiotics can give false hope or might not help. There are some early studies that suggest strong probiotics may further disrupt the balance of normal gut microbiota and make it take longer to recover after antibiotics.
Our Perspective: The gut microbiome, while poorly understood, is worth paying attention to. There is ongoing early research to support this, but it remains poorly understood. Probiotics seem generally safe when given properly. We have seen occasional anecdotal decrease in stools (number per day) in babies that have taken probiotics, as well as improvements in diaper rash (which may be related to stool output). Because research has been inconsistent between different strains or regimens of probiotics, it is too early to make a sweeping recommendation.
Here is a blog post that Dr Ted and Nurse Judy did on this topic.
Pump and Dump
What is it: Breast milk is created in the breasts by glands. Those milk-producing glands derive their nutrients from the maternal bloodstream. When breast-feeding parents ingest medications, supplements, alcohol, or other drugs, those substances can occasionally find their way into the milk. How much of that substance ends up in the milk depends on a number of factors, including the concentration of the substance in the bloodstream, how long the substance remains circulating, the size of the substance (i.e. is the molecule small enough to move through the glands), and other factors. Breastfeeding parents need to consider this when taking any substances while breastfeeding, as well as whether or not that substance is harmful to the baby.
Upside: For parents who want the absolute safest option for breastfeeding parents, using a resource to confirm breastfeeding safety is the best way to go.
Downside: Some physicians believe that we have placed too much emphasis on substance avoidance during breastfeeding (such as seen here)
Our Perspective: Every decision we make in medicine is a discussion of risk versus benefit. There is risk in taking all medications, just as there is risk in not taking medications. Below are some resources you can use for helping to make these decisions.
LactMed: A government resource that describes all the available safety literature on almost every controlled substance and medication.
MotherToBaby: MotherToBaby, a service of the non-profit Organization of Teratology Information Specialists (OTIS), is the nation’s leading authority and most trusted source of evidence-based information on the benefit or risk of medications and other exposures during pregnancy and while breastfeeding.
MommyMeds App Store/Mommy Meds Google Play: An App from Dr. Thomas Hale, a well known published physician who assigns simplified “levels” (see below) to simply describe the known safety of a medication. Medications from levels 1,2 and 5 do not need to be discussed with a clinician, unless new research emerges. Levels 3 and 4 should be discussed to appropriately consider the risk versus benefit.
L1 is super safe. It has been taken by many and has been studied
Usually the medication does not actually pass through into the milk
( it is rare to see things listed as L1)
L2 is probably safe, it has been widely used and studies have not shown any safety issues
L3 probably safe, but no controlled studies have been done
L4 potentially hazardous. But if the mom absolutely needs this and there are no other safety options, then a clear risk/benefit should be discussed with your doc
( at this point, I would say that being a good mom is not about the milk and would have mom take what she needs and put the baby on formula)
L5 Hazardous
Return to Work / Pumping Tips for Working Moms
For mom’s who need to return to a job where they will not be with their baby, it can be somewhat of a challenge to continue to breastfeed.
You can make it work!
This blog post from several years ago can help give you some strategies for helping with the transition.
Nurse Judy’s opinion. Not everyone might agree with me but once a mom goes back to work, trying to continue to EXCLUSIVELY breastfeed can be stressful. (understatement)
My recommendation is to nurse and pump as much as you can reasonably do, but also to figure out if there is a formula supplement that your baby tolerates well. Simply having that option can decrease the stress levels enormously.
Some moms are surprised to hear me tell them that my sweet spot is 80% breastmilk and 20% formula. That little bit of formula might mean that you get a nap!
It can also keep you from having an anxiety attack if a meeting goes longer or you are stuck in traffic.
Silverettes
What are they: Protective shield made of silver that provides a barrier between the nipple and clothing. Silver is naturally antimicrobial and antifungal. It is purported to contain potent anti-inflammatory properties.
Upside: Silverettes can protect the nipples! We want to do everything we can to decrease barriers to breastfeeding, and pain is a big barrier.
Downside: Silverette’s aren’t dirt cheap. They represent an added cost, and they can get lost.
Our Perspective: For those who can access them, either through buying or being gifted them, silverettes can be a tool to keep breastfeeding comfortable, and they have no documented downsides of which we are aware.
Sunflower or Soy Lecithin
What is it: lecithin refers to different emulsifying components of human milk. The components already exist in human milk, but some mothers may take large doses of supplemental lecithin from the sunflower or soy plants. As an emulsifier, lecithin thins milk.
Upside: Lecithin products such as sunflower lecithin are part of the American Academy of Breastfeeding Medicine’s 2022 Clinical Protocol for Mastitis. They are an option to reduce inflammation and pain, alongside ice, Advil, and breast rest. They may be very helpful for overcoming recurrent mastitis, particularly in people with dense breast tissue. They specifically work to break down biofilm plaques in people with dense breast tissue
Downside: Lecithin products do make it directly into breast milk and into babies. While we do not suspect this is a problem (again, lecithin exists in breastmilk currently) we do not know the impact of altering the ratio of breast milk emulsifiers on baby’s health. There have been no studies or case reports to suggest any harm or downside.
Our Perspective: All breasts and babies are different. Sunflower or soy lecithin (5–10g daily by mouth) seems appropriate for some people with some kinds of mastitis, and is included in the 2022 Academy of Breastfeeding Medicine Guidelines. For the average person, it is not necessary to start with a lecithin supplement, but because it is hard to determine the kind of mastitis somebody has, lecithin seems to be safe as an option for people with recurrent mastitis.
Tongue Tie (and Tongue Tie Revision Procedures)
What is it: A “tongue tie” is extra tissue that makes it difficult for a person to move their tongue – there are also both “posterior” and “anterior” versions which affect the appearance of the tongue as well as its function. There are also lip ties attaching the lips to the gums, and buccal ties attaching the cheeks to the jaw. In some cases, these can make breastfeeding painful for breastfeeding parents and milk transfer difficult for some breastfeeding babies, and can sometimes affect bottle feeding as well. In some cases, it can have effects later in life such as impairment of speech development and need for orthodonture. Tongue ties (and lip and buccal ties) can be “revised” (clipped) by a pediatric ENT using tiny scissors or a pediatric dentist using a specialized laser.
Upside: If the ties are severe and treated early, it can make breastfeeding much easier and more effective, as well as prevent any future negative effects. Breastfeeding a severely tongue-tied baby can sometimes be painful for the breastfeeding parent, and holding one’s baby at a different angle does not always solve it. Early on, tongue tie repair has an easier recovery process for the baby. An older child or adult might need to have a tongue tie procedure under general anesthesia, but it’s a fast outpatient procedure (seconds to minutes) for infants.
Downside: It’s a procedure on a baby, and the baby will experience pain. The baby can be given painkillers. There may be a cost associated with the procedure (medical or dental insurance). While there is anecdotal evidence that tongue tie repairs help some babies and parents, there are only a few small randomized controlled trials showing this, and the benefits in those studies have been modest.
Our perspective: Just like some pregnancies are easy and some are difficult, not all ties are created equal! Some babies (and breastfeeding parents) may benefit significantly from a tongue tie revision procedure and others may experience little benefit. Procedures are more easily tolerated by the baby the earlier they are done earlier. While IBCLCs, pediatricians, ENTs, and pediatric dentists can all weigh in on “is it a real tongue tie,” finding a provider in the local area who does a lot of tongue tie revisions may give the parent more clarity in ruling out whether a tongue tie procedure is likely to provide benefit.
Weaning and Hormone Shifts
Two of the hormones that directly affect breastfeeding are prolactin and oxytocin. Oxytocin can create feelings of warmth and closeness. Prolactin can make people feel calm and relaxed.
When you wean, those ‘feel good’ hormones are about to precipitously dip.
Mom’s wean for any number of reasons. It is rarely a simple decision. Even though it means you can regain body autonomy, for most moms there are a lot of mixed feelings. This is normal.
So, not only are you dealing with complex emotions, you also have hormonal shifts
Knowledge is power. When you understand that there is a physiologic reason for feeling some imbalance, it might make it a bit easier to deal with.
Wounds / Abscess
What are they: This is an entry for open wounds (not mastitis spectrum, not “clogged ducts”). We are referring to nipples that are excoriated, scabbed, are bleeding or have pus. Wound healing can take one of two high-level approaches: either the healing occurs open to the air or covered.
A breast abscess is a painful, swollen lump in the breast that may be red, warm to the touch, and sometimes accompanied by fever or flu-like symptoms. If you’ve developed an abscess, it’s important to seek medical attention.
Upside: Surgeons in the field of breastfeeding medicine recommend keeping open skin wounds covered and moist, such as with hydrogel pads (see below). This is in line with most dermatologic research on optimal healing for wound care.
Downside: Other interventions, such as epsom salt soaks, use of nipple shields, keeping breasts open to the air, and use of black tea bags all have years of use with experienced lactation consultants. However, their use is not consistent with research on optimal wound care, and some providers believe that they carry some risks for parent and baby.
Our Perspective: Nipple wounds should be lubricated and covered to heal effectively, just like burns or other open wounds on the body. An organic balm coupled with a hydrogel “soothie” pad to “close” the wound can be utilized. Moms should keep nipples covered both day and night to enable uninterrupted wound healing.
Vasospasm
What is it: The breast has a lot of blood vessels. Those vessels have muscles around them, which may constrict in response to stimulation, such as by the breasts filling with milk or the baby latching. This constriction can cause a sharp pain, described as a “zingy” sensation, like electricity. It doesn’t necessarily need to happen during feeding or let down, it can happen at any point.
What can help: This kind of pain is different from the inflammation from mastitis pain, and so it should be treated differently. Warm compresses can be very helpful, or any way of applying heat. Changing a baby's latch position can sometimes be beneficial to avoid further inciting the constricted vessels.
Volumes and Feeding Times
What is it: Prescribing specific timing or amounts for breastfeeding and supplementation after discharge from the hospital (i.e. feed for X minutes and supplement with Y mL of formula or pumped milk.
Upside: Newborn care can feel overwhelming, and so providing specific numbers helps data-oriented parents to know what to do.
Downside: Every baby and breast is different, so while one baby might need 15 minutes to drain a breast, another might need 10 minutes, and supplementation varies based on baby/stomach size and hunger needs. Giving specific timing is well intended, but recognizing hunger cues is better practice.
Our Perspective: Overly prescriptive plans (i.e. do exactly X minutes per breast at Y interval) ignore the unique makeup of every breast and baby. Talk to your clinical team about how to recognize hunger cues. If you have questions about whether or not you’re feeding your baby enough, ensure they have adequate wet diapers and are getting weighed by their pediatrician as they deem appropriate. If your baby is calm, awake, and looking around, they’re usually doing just fine!
Yeast
What is it: Candida albicans, or yeast, lives in warm dark moist places and feeds on simple sugars (i.e. breastmilk). Many maternal biomes have evidence of candida, both in the vagina, the poop, and sometimes in the breast. It is a natural part of normal flora, but can be problematic if it divides out of control in those warm dark moist places. This entry focuses exclusively on treating the breastfeeding nipple. There is generally strong and uncontroversial guidance to treat babies with nystatin when thrush is appropriately diagnosed (usually visualized by a clinician).
Upside: Practitioners who believe in treating yeast state that it’s very safe to do. There are many options, such as treating baby and mom with topical nystatin, leaving breasts out to dry, or applying gentle nipple creams, that breastfeeding parents can use.
Downside: Some practitioners strongly believe that yeast is incapable of living on nipple surfaces. They also state that the risk of harm to the nipple with some treatments outweighs the benefits.
Our Perspective: There are a lot of conflicting opinions and minimal data to help guide the decision of whether or not to treat nipples for yeast. Still, there are very low risk interventions that parents can use to keep nipples healthy. Air to the nipples is great (keeping breasts out of a bra to dry). If there is a decision to treat mom’s nipples with a bland nipple cream, do not wash off the cream after application. Instead, wipe with a neutral tissue. The soap and water involved with washing the nipples can cause pain/discomfort/cracking.
Products that we like
The list below are not essential to a successful breastfeeding journey, and we don’t like recommending any one product over another. These are just things that parents have used and liked, so we’re sharing the love.
Silverettes
Bamboo breast pads
Medela Manual Breast Pump
Special shout out to:
Julie Hartman is a Certified Lactation Counselor, certified Birth Doula, and new parent educator.
Dr. Ted Handler is a pediatrician in the East Bay with a passion for lowering the temperature on hot debates in medicine.
Nancy Elle who helped design the document to make it easier to read and search.
Lauren Kivowitz who added her real life experience as a nursing mom. She was the catalyst behind our decision to expand and publish our original document. I forgive you for your nursing strike at 4 months old. Seeing you as such a wonderful mom fills my heart.
Ellie Powers who was on our Oath team and worked with us on the document the first time around as well as this one. Her perspective as a mom who faced many of the challenges mentioned above was invaluable.
Thanks to all of the moms who sent it their input and suggestions for topics to cover. If we didn’t get to it, our apologies, we came to the realization that if we strived for something that was perfect and complete, we would never be ready to send it out
Hugs to all the parents out there who are doing the best they can!
This document was a labor of love.
We have decided to make it free to everyone. If you found it useful, pay it forward: do something positive in the universe or do something nice for a new parent.
If you know someone who is breastfeeding, feel free to share.


No comments:
Post a Comment