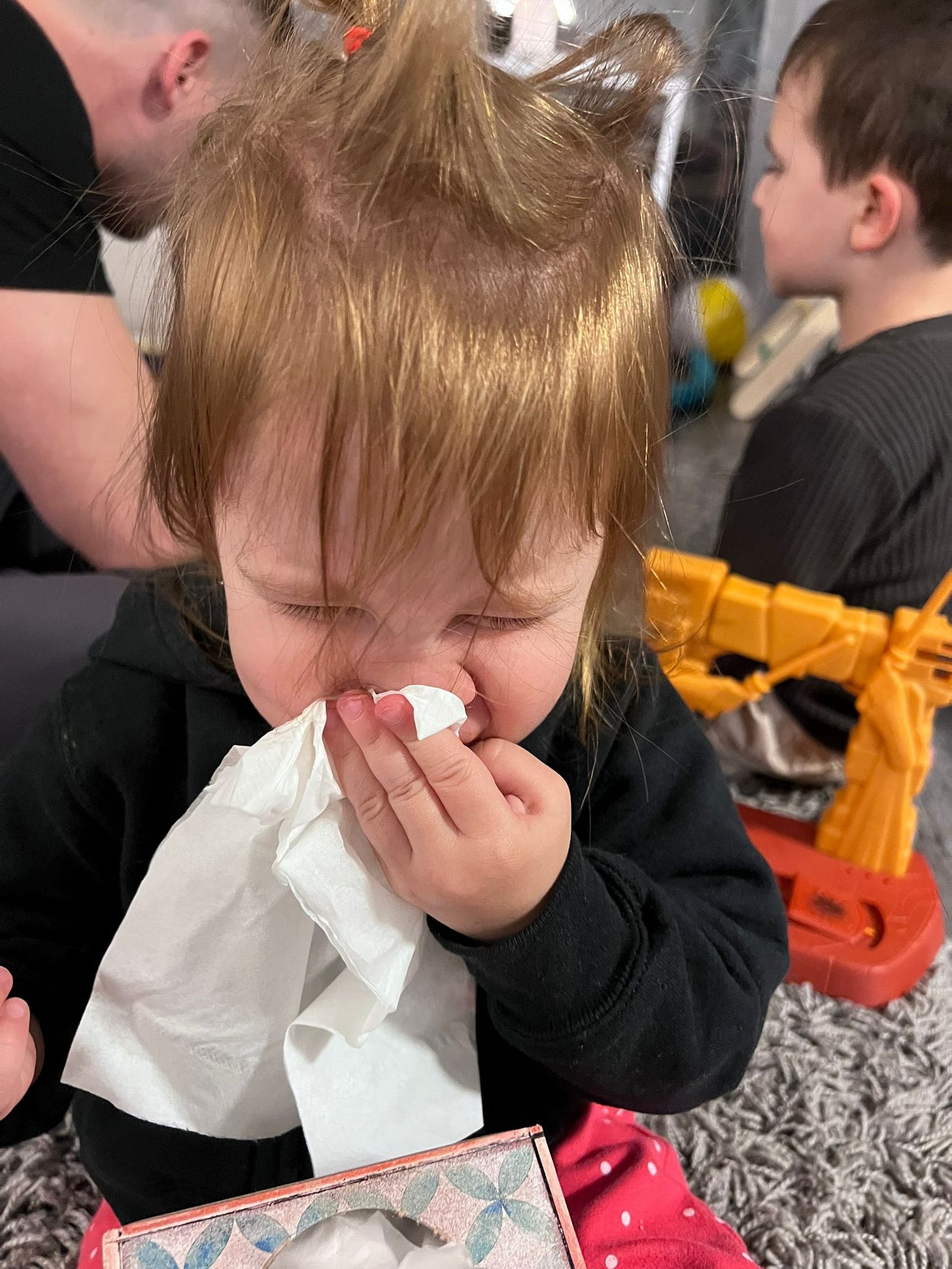
One of the wordle answers this week was FEVER. That same day my grandson Elliot needed to stay home from preschool because he had an elevated temperature.
For everyone who doesn’t have a grandma on speed dial, here is the blog post that can answer all of your fever questions.
Everything you need to know about Fevers
Fevers tend to get parents very worried, but an elevated temperature is only one of the factors that you need to consider when evaluating a sick child. I am actually more interested in your child's overall mood and behavior than I am in any specific number on a thermometer.
An adult with a high fever is usually more miserable and needs to be evaluated sooner to figure out what is going on.
For kids, fevers are a right of passage. There are advantages for them to get all the common illnesses out of the way when they are young. Most of these offer some degree of immunity so they don’t catch them when they are adults. All of you parents who caught hand foot mouth from your kids because you somehow avoided it growing up, are nodding vigorously.
There are many methods out there for measuring body temperature. I personally don't feel the need to invest in any expensive thermometers. I am generally quite satisfied with digital underarm reading. The important thing is that however you measure it, your thermometer seems accurate. Test it on yourself or other family members and take your child's temp when they are healthy to make sure you trust it as well as to establish what the normal baseline is for your child. While 98.6 is considered an average ‘normal’ temperature. Some people run a little hotter or colder.
Here are a couple of links that give a good description of some of the thermometer options
https://www.nytimes.com/
https://www.health.com/
Years ago when I was still working in the pediatricians office, ear thermometers were notorious for giving absurdly high and inaccurate readings that would induce panic in their parents. The newer generation of devices may be more accurate, but keep the following in mind:
If your child looks quite ill and the high temperature correlates with symptoms, then take appropriate action.
If your child looks fine, please don't let a number on the thermometer freak you out. Instead, take a deep breath and look at your child! If they are grinning at you and singing, that is not someone I am terribly worried about.
Temperatures can be measured in either Fahrenheit or Celsius
Here is a quick conversion chart.
98.6 F=37 C
99.5F=37.5C
100.0F=37.8C
100.4F=38C
101F=38.4C
102F=38.9C
103F=39.5C
104F=40C
105F=40.6
For this post, I will be referring to the temperatures on the Fahrenheit scale.
However you take it, the route of measurement is important data to your reporting. 99 degrees under the arm is not quite the equivalent to 99 degrees rectally. Axillary temps can be roughly a degree lower on some kids. It is still perfectly fine to use the underarm method. Most of the time we are just getting a sense of the range. There is no clear consensus, but most doctors would consider any temp below 100.4 to be low grade.
For any child older than 3 months
As long as your child is active and happy, I generally don't feel the need to "treat" a fever unless it is over 101.5 or so.
I am much more concerned about the lethargic, whimpering child who has a normal body temperature than I am the singing child with 104. But, here is……
“Nurse Judy's rule’ about fevers:
If the fever is over 102 (it doesn't matter how you measure, just be consistent):
Treat with proper dose of Acetaminophen or Ibuprofen
Do a tepid bath or place cool compresses on the forehead, insides of elbows and neck
This is not the time for fuzzy pajamas!
Get them drinking. Little sips at a time are fine. A Popsicle or ice-chips are good for older kids.
If you have a stash of breast milk, you can offer a ‘milksical’. Put frozen milk in one of the mesh feed bags and Voila.
When we are trying to push fluids, adding a little splash of juice to their water is perfectly fine at this point; you are doing whatever you can to get the hydration going.
re-check the temp in 45-60 minutes. We want to see some improvement by the 45 minute mark, but it can take 90 minutes before you get significant improvement.
If the temperature is STILL over 102 after the medication and hasn't budged at all, we are dealing with a fever that needs to be evaluated.
If a fever higher than 101 degrees lasts for more than 3 days, even with a happy child, I consider it time to have a look so that you can make sure there isn't an infection source (like ear infection, urinary tract infection, strep throat or pneumonia.)
I would allow five days for low grade temps before taking them in.
Fussy kids who are inconsolable need to be seen sooner than that, fever or not.
During flu season, sometimes there are kids with fevers that are hanging on for five days or longer. If there is a known virus actively circulating in your area, your doctor may be okay ‘watching and waiting’ for another couple of days before asking you to come in for a visit. This would likely depend on if your little one is managing (drinking, peeing, easy breathing, consolable, fever responds to medications.)
Many viral syndromes "wave goodbye" with a rash. Roseola is a classic example. When I have a happy kid with a high fever, it is pretty common at day three for the fever to be gone. Now you have a fussy kid with a rash on your hands, but you also have an answer.
https://nursejudynvp.blogspot.
Time is the great fixer here, there is no need to be seen.
With most rashes, including roseola, when you push on the skin the area should lighten. This is called blanching. A purple rash that does not get lighter when you press is always worth calling your doctor about. Any fever that comes along with a purplish rash could be an emergency like meningitis. Don’t wait to be seen.
I remind you that your child’s activity and energy level are still the biggest clues. Generally with something serious it is clear that something is wrong. These kids are not running around babbling and playing. They are sick, and it is obvious.
It is useful for you to know that when children are in the process of spiking a fever, it is not uncommon for them to tremble and look shaky. This is normal.
Children with fevers may have a higher respiration and pulse rate.
When fevers are breaking it is common to have lots of sweating. They can soak right through the sheets!
It is also important to be aware that about 4% of children can have something called a febrile seizure. This is not the same as the trembling that I mentioned above.
Febrile seizures can be terrifying to watch, but they usually stop within 5 minutes. They cause no permanent harm. Trust me, if you have never heard of this, watching your child have a seizure has been reported as the scariest experience EVER.
Having the prior knowledge that they do happen once in a while and are generally harmless should help keep you from freaking out. If your child is having a seizure they may have large jerky motions and their eyes may roll back. Make sure their airway is open. It is perfectly reasonable to call 911. Your job is to stay calm.
If your child has had even one febrile seizure, your medical team is likely to be more aggressive with fever control and might advise you to treat even a low grade fever. It is important to talk with your doctor about this so that you have a plan in place that you are comfortable with. Fortunately, most kids grow out of seizures by the time they are 5 years old.
If your infant is under 3 months of age, it is important to pay much closer attention to any elevated temperature
Where infants are concerned, there are a few common causes:
*over bundling....
Seriously, When I was working at Noe, sometimes the new babies would come into the office with piles of blankets wrapped around them even on a warm day. I know that many of us have the tendency to bundle up an infant but the best rule of thumb is to dress them in one layer more than you are wearing. If your baby was indeed over bundled, get some of those layers off and re-check the temp in about 10 minutes to see if they have cooled down.
*dehydration...
Sometimes if mom's milk isn't in yet, babies can be simply dehydrated and need to get some fluids. This is the time that you need to squirt some milk or formula directly into your baby's mouth. You can use a syringe or a dropper. In some cases the elevated temperature will normalize fairly quickly from some fluids.
If there is no obvious cause for an elevated temperature, and it doesn't resolve within 15 minutes, your baby needs to be evaluated. Giving a fever reducing medication to a newborn should only be done under strict guidance from your pediatrician.
With the younger babies, it is always better safe than sorry. Certainly there is no down side for calling and checking in with your doctor just to be on the safe side.
Some general fever facts:
Fevers turn on the body immune system. They are one of our body's protective mechanisms
Many fevers can actually help the body fight infection.
Fevers that are associated with most viral syndromes and infections don't cause brain damage. Our normal brain's thermostat will not allow a fever to go over 105 or 106.
Only body temperatures higher than 108°F (42.2°C) can cause brain damage. Fevers only go this high with high environmental temperatures (e.g., confined to a closed car.)
Bonus tidbits from Dr Ted:
I have to reiterate everything that Nurse Judy has said above! Fevers are a difficult concept for a lot of parents to wrap their heads around, especially the first time they see one. It’s useful to remember that everybody’s immune system is different, and the exact same virus can cause a fever to 104 in one kid and pass without symptoms in another. An increase in body temperature is the body‘s response to “inflammatory cytokines“, chemicals released by your body's healthy tissues when they are under stress, like being attacked by a virus. Some bodies release more of these chemical signals than others, which is why different bodies have different temperatures to the same viruses. Immune systems also have different abilities to fight off different viruses within the same family, which is why some viruses pass without any symptoms at all in some children and the same virus can wreak havoc in others.
Parents always asked me, “At what temperature do I panic?“ My answer is 106. If you can trust that your child’s temperature is truly at or above 106, using Nurse Judy‘s techniques above, you must go to the emergency room. Anything below that is a question should be based on the child’s appearance.